Understanding Overactive Bladder: Causes, Symptoms, and Treatment Options
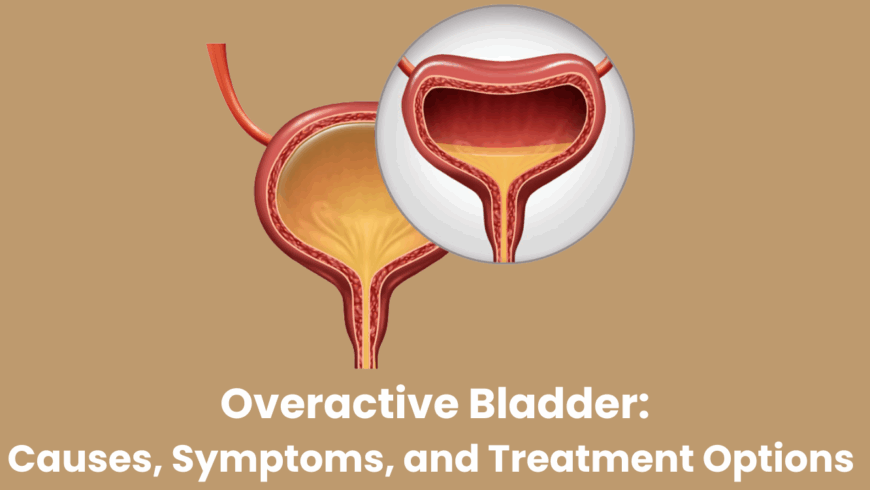
Overactive bladder (OAB) is a common yet often overlooked condition that significantly affects the quality of life, especially among women. It is characterized by a sudden, uncontrollable urge to urinate, often accompanied by increased frequency and even leakage. While not life-threatening, OAB can lead to embarrassment, anxiety, and social withdrawal if left untreated.
If you or someone you know is facing such symptoms, consulting a gynecologist in Hadapsar like Dr. Pallavi Mulay at Mulay Hospital can provide clarity, diagnosis, and effective treatment.
What is Overactive Bladder?
Overactive bladder is a condition that involves problems with bladder storage function. The hallmark symptoms include:
-
Urinary urgency: A sudden and strong urge to urinate.
-
Frequency: Needing to urinate more than eight times in 24 hours.
-
Nocturia: Waking up more than once at night to urinate.
-
Urge incontinence: Involuntary loss of urine immediately after feeling a strong need to urinate.
OAB is not a disease, but a group of urinary symptoms. It can affect both men and women but is more commonly reported among women, especially as they age or go through hormonal changes such as menopause.
What Causes Overactive Bladder?
There is no single cause for overactive bladder, but several factors can contribute to its development:
1. Muscle Overactivity
The bladder muscle (detrusor) contracts involuntarily, even when the bladder is not full. This abnormal muscle activity leads to urgency and frequent urination.
2. Neurological Disorders
Conditions such as multiple sclerosis, stroke, Parkinson’s disease, or spinal cord injuries can affect nerve signals between the brain and bladder, leading to OAB.
3. Hormonal Changes
Post-menopausal women often experience changes in estrogen levels, which may weaken the bladder lining and pelvic muscles, making OAB symptoms more prominent.
4. Urinary Tract Infections (UTIs)
Although not a direct cause, UTIs can mimic or exacerbate OAB symptoms.
5. Lifestyle Factors
High caffeine or alcohol intake, constipation, and obesity are known to aggravate overactive bladder symptoms.
Who is at Risk?
-
Women over the age of 40
-
Individuals with diabetes or neurological disorders
-
Pregnant women or those who have recently given birth
-
Women in the post-menopausal phase
If you’re experiencing any of these symptoms and fall into a high-risk category, it’s advisable to consult an experienced gynecologist in Hadapsar for a thorough evaluation.
How is Overactive Bladder Diagnosed?
Diagnosis typically involves a detailed medical history, physical examination, and certain tests such as:
-
Urinalysis to rule out infections or blood in the urine
-
Bladder diary to track the frequency and volume of urination
-
Ultrasound or urodynamic testing to assess bladder function
Your gynecologist may also check for other underlying conditions like pelvic organ prolapse or fibroids that could be influencing your symptoms.
Treatment Options for Overactive Bladder
OAB can be effectively managed with a combination of lifestyle changes, medications, and in some cases, surgical intervention. The treatment approach is usually tailored to the severity of the condition and individual patient needs.
1. Lifestyle Modifications
-
Bladder training: Delaying urination gradually to increase bladder capacity
-
Pelvic floor exercises (Kegels): Strengthening the muscles that control urination
-
Dietary changes: Reducing intake of caffeine, alcohol, and spicy foods
-
Weight loss: Even modest weight loss can reduce pressure on the bladder
2. Medications
Anticholinergic medications and beta-3 adrenergic agonists are commonly prescribed to relax the bladder muscle and reduce urgency and frequency.
3. Physical Therapy
Pelvic floor physiotherapy has shown excellent results in improving muscle control and reducing leakage episodes.
4. Advanced Therapies
For severe cases that do not respond to conservative treatment, options may include:
-
Botox injections in the bladder muscle to reduce overactivity
-
Nerve stimulation therapy such as sacral neuromodulation
-
Surgical procedures to enhance bladder capacity or control
Dr. Pallavi Mulay provides a patient-centered approach, ensuring that every woman receives care tailored to her needs and comfort.
Living Well with OAB
Although OAB can feel like a burden, many patients experience significant relief with the right treatment and support. It’s essential to approach the condition with a proactive mindset rather than embarrassment or hesitation. Seeking timely consultation and adhering to prescribed treatments can dramatically improve your daily comfort and self-confidence.
At Mulay Hospital, compassionate care and advanced gynecological expertise come together to support women dealing with overactive bladder and other urogynecological concerns.
Overactive bladder may be a common issue, but it shouldn’t be ignored. With increasing awareness, modern diagnostics, and effective treatments available, women no longer have to accept urinary urgency and frequency as a normal part of aging or motherhood.
If you’re struggling with symptoms of OAB, book an appointment with Dr. Pallavi Mulay, an experienced gynecologist in Hadapsar, and take the first step toward better bladder health and a better quality of life.